What is PR2 in Medical Billing?
Medical billing involves complex processes to manage healthcare payments efficiently. Insurance companies use specific codes to explain claim payment decisions clearly. One important code in this system is known as PR2. Understanding PR2 helps providers and patients handle payment responsibilities properly. This article explores the meaning and significance of PR2 thoroughly.
PR2 is a remark code used in Explanation of Benefits statements. It specifically indicates patient responsibility for deductible payment amounts. Deductibles are the initial out-of-pocket expenses patients must cover annually. When a patient hasn’t met their deductible, PR2 clarifies the owed balance. Accurate knowledge of PR2 helps streamline billing and patient communication.
Healthcare providers rely on PR2 to identify unpaid deductible portions from patients. Insurance carriers apply PR2 to claims when deductibles remain unmet. This ensures transparency between insurers, providers, and patients regarding payment. Medical billers use PR2 to manage accounts and follow up efficiently. Knowing PR2 is essential for smooth medical billing operations.
Table of Contents
What Does PR2 Mean in Medical Billing?
PR2 is a patient responsibility code for deductible amounts owed by patients. It explains why insurance denies certain payments to healthcare providers. When a deductible is not met, PR2 applies to claims. This code helps clarify patient financial obligations clearly and concisely. Understanding PR2 is vital for accurate medical billing processes.
Deductibles are the initial amounts patients must pay annually themselves. Only after reaching deductibles does insurance cover remaining healthcare costs. PR2 reflects the part of the bill patient must cover first. This prevents confusion between provider, patient, and insurance payer. Providers rely on PR2 to collect accurate payments promptly.

PR2 also appears on Explanation of Benefits or Electronic Remittance Advice. These documents outline how insurance processed the submitted medical claim. Providers use PR2 codes to determine which amounts are patient responsibility. It aids billing departments in preparing correct patient statements. Therefore, PR2 is critical for transparent healthcare financial communication.
Understanding Patient Deductibles and PR2 Responsibilities
Deductibles require patients to pay a specific amount before insurance coverage starts. PR2 indicates the patient must pay this deductible portion before benefits apply. This code ensures the provider knows the patient’s financial responsibility clearly. Understanding deductibles helps patients prepare for out-of-pocket healthcare expenses.
Patients often find deductibles confusing without clear explanations from providers or insurers. PR2 on statements helps clarify why certain charges aren’t covered by insurance. Providers can educate patients about deductibles during visits or billing processes. This transparency builds trust and reduces payment delays significantly.
How PR2 Affects Healthcare Providers and Patients

PR2 impacts providers by identifying deductible amounts owed by patients. It helps providers bill patients correctly and avoid financial losses. Without PR2, providers might incorrectly assume insurance will pay everything. Accurate application of PR2 reduces confusion during patient collections. This improves overall revenue cycle management and cash flow.
For patients, PR2 provides clear explanations about payment obligations. It informs them why certain charges are their responsibility. Many patients misunderstand deductible concepts until they see PR2 codes. Proper education around PR2 improves patient satisfaction and trust. Providers can also arrange payment plans based on PR2 information.
PR2 also influences insurance claim processing timelines and accuracy. Insurance companies send PR2-coded remittances to detail deductible application. Billers use this data to adjust claims and patient balances. Timely follow-up on PR2 claims helps reduce outstanding patient debt. It keeps billing systems accurate and compliant with payer guidelines.
Role of PR2 in Explanation of Benefits (EOB)
Explanation of Benefits documents provide detailed information on claim payment results. PR2 appears on EOBs to show amounts the patient owes from deductibles. Providers and patients rely on these explanations to understand claim adjustments clearly. EOBs with PR2 help prevent misunderstandings about insurance payment responsibilities.
Insurance companies send EOBs after processing claims, highlighting patient responsibility codes. PR2 specifically explains why part of the claim isn’t paid by insurance. Billers use this information to adjust patient statements and follow up efficiently. This clarity reduces confusion during the billing and payment cycle.
Impact of PR2 on Medical Billing Workflow
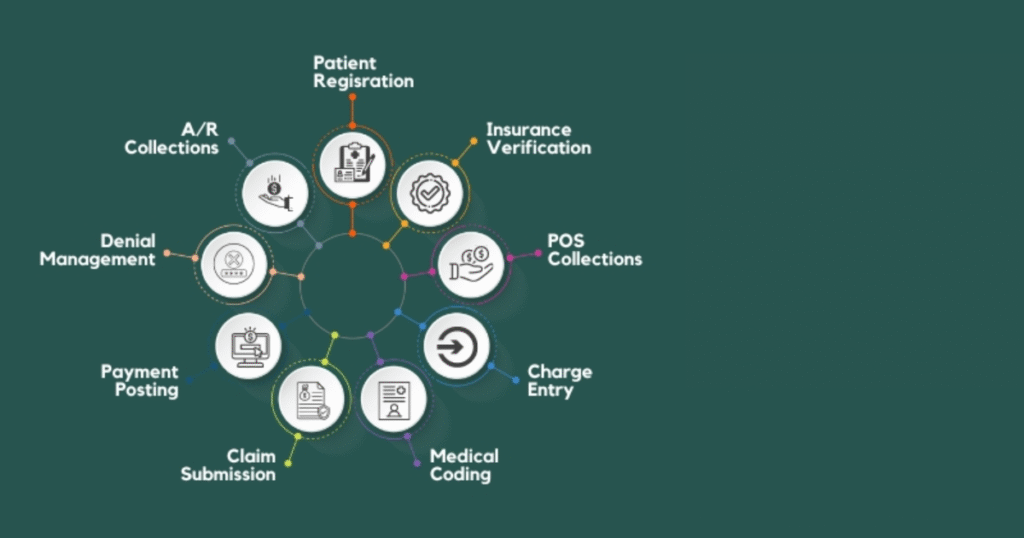
PR2 codes prompt medical billers to accurately bill patients for deductible amounts owed. This helps providers avoid writing off amounts that should be collected from patients. Efficient management of PR2 claims improves overall revenue and reduces outstanding balances. Medical billing software often flags PR2 for easier tracking and collections.
Handling PR2 requires communication between insurance companies, providers, and patients. Timely follow-up on PR2 balances prevents delays in payment collection processes. Providers benefit from setting up automated reminders for outstanding deductible amounts. Proper workflow management with PR2 enhances financial stability in healthcare settings.
Best Practices for Managing PR2 in Medical Billing
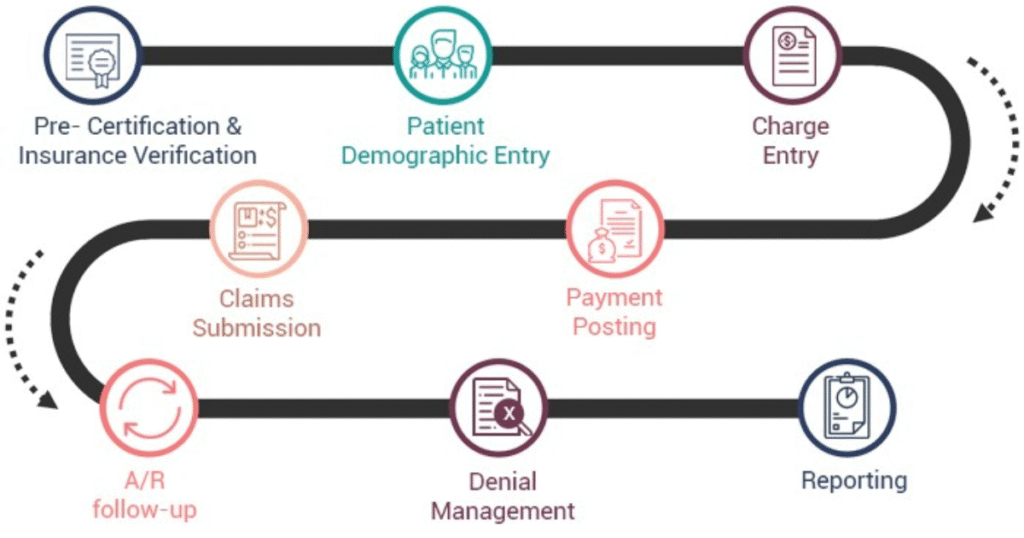
Providers should verify deductible balances before billing patients with PR2 amounts. Accurate verification prevents billing errors and patient disputes later on. Medical billing software often integrates PR2 data for streamlined processing. Automation reduces manual mistakes and improves billing accuracy significantly. Keeping updated patient deductible information is essential for success.
Clear communication with patients about their deductible responsibility is critical. Providers should explain PR2 and its impact during visits or billing. Transparent communication encourages timely patient payments and fewer outstanding balances. Sending detailed patient statements including PR2 codes helps avoid confusion. Educated patients are more likely to cooperate with payment requests.
Providers must track PR2 codes carefully to optimize collections efforts. Monitoring PR2 allows for identifying unpaid deductible balances efficiently. Setting up reminders for patient follow-ups on PR2 amounts improves cash flow. Coordinating with insurance companies ensures proper claim adjustments are made. Implementing these strategies leads to smoother revenue cycles overall.
Common Challenges and Solutions Related to PR2
One challenge is patients misunderstanding their deductible responsibilities indicated by PR2 codes. This can lead to delayed payments or disputes about amounts owed. Providers can overcome this by offering clear explanations and patient education resources. Effective communication minimizes confusion and encourages timely payment compliance.
Another challenge is tracking deductible balances accurately across multiple claims and payers. Errors in tracking can result in incorrect billing and frustrated patients. Utilizing advanced billing software that integrates insurance data helps resolve these issues. Accurate tracking of PR2 ensures smooth billing and improves patient satisfaction.
- PR2 indicates patient responsibility due to unmet deductible amounts on claims.
- Deductibles are annual out-of-pocket amounts patients pay before insurance coverage starts.
- Accurate use of PR2 helps providers avoid billing errors and payment delays.
- Medical billing software often flags PR2 codes for efficient deductible tracking.
- Educating patients about PR2 and deductibles encourages timely payments and reduces confusion.
Conclusion
Understanding PR2 is essential for accurate medical billing and collections. It clearly defines patient responsibility related to deductible amounts owed annually. Providers rely on PR2 to communicate financial obligations to patients effectively. This reduces confusion and improves timely payments from patients significantly. Mastering PR2 helps optimize revenue cycles and financial stability.
Effective communication about PR2 codes builds trust between patients and providers. Educating patients on deductibles and payment responsibilities encourages cooperation and clarity. Transparent billing processes reduce disputes and increase patient satisfaction overall. Providers benefit from explaining PR2 during visits or billing statements. This approach fosters better healthcare financial experiences for everyone.
Accurate tracking and management of PR2 improve billing workflow efficiency greatly. Automation in billing software helps identify and follow up on deductible balances. Timely collection of PR2 amounts supports steady cash flow in practices. Healthcare organizations should prioritize understanding and applying PR2 codes correctly. Doing so ensures smoother financial operations and fewer payment delays.
FAQ’s
What does PR2 mean in medical billing statements?
PR2 means patient responsibility due to an unmet deductible amount.
When is the PR2 code applied to a medical claim?
It is applied when the patient has not met their deductible yet.
How does PR2 affect the patient’s payment obligations?
Patients must pay the deductible amount before insurance covers additional costs.
Can providers collect deductible payments directly after receiving PR2?
Yes, providers bill patients for the deductible indicated by the PR2 code.
How can medical billers track PR2 amounts efficiently?
Using billing software that integrates insurance data and flags PR2 balances.
Leave a reply